Periodontitis
- Diagnosis
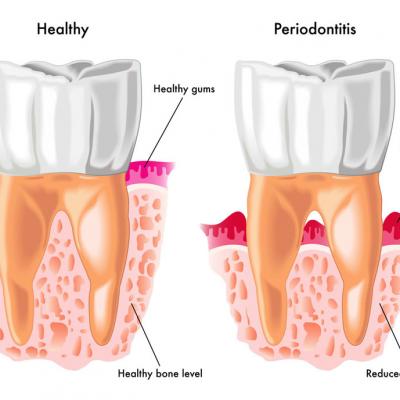
Periodontitis is an inflammatory disease affecting the supporting tissues of the teeth (gingival, alveolar bone and periodontal ligament). It affects a large percentage of the adult population (about 40%). Periodontitis is caused by bacteria normally present in the oral cavity and it manifests when the conditions present allow for the multiplication of these microorganisms. As microbial numbers increase, the inflammation intensifies, resulting in the destruction of the supporting bone and recession of the gums.
Patients initially do not present with symptoms other than bleeding of the gums, which itself might be masked by smoking, and frequently the disease goes undetected until the gums start receding, halitosis (bad breath) appears and the teeth become loose. Diagnosis requires a special clinical and radiographic examination and the patients are referred to a specialist periodontist by their general dental practitioner. Periodontal disease may progress at a slow rate (Chronic Periodontitis) or present with rapid bone loss (Aggressive Periodontitis).
At the initial examination, the periodontal specialist performs special measurements around each tooth (periodontal charting), in order to determine the degree of attachment loss. Radiographic (x-ray) examination is required in order to confirm the diagnosis and formulate the treatment plan. These clinical measurements are repeated at least 6 weeks following the treatment and at the maintenance visits.

- Periodontal therapy
Oral hygiene instruction:The basic requirement for a successful treatment is proper oral hygiene. Prior to the treatment, the level of oral hygiene performed by the patient is assessed and instructions are given, according to the needs of each patient. A proper brushing technique is demonstrated alongside with the use of interdental cleansing means. Good oral hygiene helps with inflammation control and assists healing of the gums. It is therefore of utmost importance in the treatment of periodontitis as well as in the maintenance of a good result. Oral hygiene levels are frequently checked and instruction is repeated if necessary.
Non-surgical periodontal therapy
- (α) (a) Initial treatment: Initially, a cleaning of the teeth (scaling) is performed above and under the gums, in order to remove all calculus deposits from the teeth and reduce the microbial counts as much as possible. Scaling is performed with the help of ultrasonic and hand instruments. The treatment is completely pain-free, performed under local anaesthesia. Following the treatment, most patients experience minor discomfort which, in the majority of cases, does not require the use of painkillers. In some cases, depending on the severity and the aggressive nature of the disease, antibiotics are prescribed.
- (b) Reassessment and final treatment plan: At least 6 weeks following initial therapy, re-evaluation is performed, in order to assess the outcome of the treatment. In case residual periodontal pockets are present, treatment continues with either the repetition of non-surgical therapy or with a surgical approach, if necessary. In many cases, pocket reduction is achieved by the initial treatment and no further active therapy is required. The patient then enters a program of supportive periodontal therapy, with regular checkups and professional cleaning.
Periodontal surgery: This second phase in the treatment of periodontitis is performed in cases where, following non-surgical treatment, residual pockets which cannot be reduced by a second round of non-surgical are present. This may be due to lack of access to the areas of interest, very deep initial pockets or in case one of the various regenerative techniques must be performed. The goal of surgical therapy is to create a healthy environment which can be maintained clean by the patients themselves with the use of oral hygiene means at home. Surgical periodontal therapy is performed under local anaesthesia and, provided the patients have a good level of oral hygiene and surgery is performed following the initial infection control, healing is generally uneventful. Minor complications may arise including swelling, bruising and discomfort or mild pain which is managed with over-the-counter analgesics.
- Supportive periodontal therapy
Supportive periodontal therapy: Following successful periodontal treatment, patients enter a program of maintenance therapy. This includes 3, 4 or 6-monthly visits for a clinical periodontal examination, oral hygiene reinforcement and professional scaling and polishing. Supportive therapy aims at the maintenance of the good treatment result and the prevention of disease recurrence. Depending on tooth sensitivity, scaling may be performed with or without local anaesthesia.
The success of any periodontal therapy is highly dependent on patient compliance. Good oral hygiene and regular maintenance visits are essential for a satisfactory and long-lasting treatment result.